
She is responsible for creating, editing, and managing all content, design, and interaction on the company website and social media channels in order to promote CIPROMS as a thought leader in healthcare billing and management.įor more information about how we use your data, please review our privacy policy.
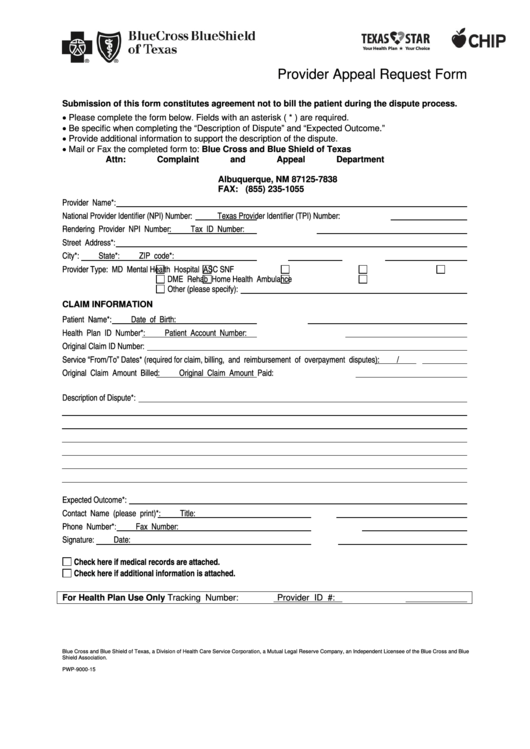
Charity Singleton CraigĬharity Singleton Craig is a freelance writer and editor who provides communications and marketing services for CIPROMS. Note: You must provide supporting documentation with this request. Please use this form to request a review of your or your patient’s contractual timely filing limit. For use or reprint in your blog, website, or publication, please contact us at. REQUEST FOR TIMELY FILING REVIEW We will consider circumstances beyond a provider’s or members control that resulted in delayed submission of claims on a case-by-case basis. All claims that do not involve other insurance must be received by TMHP within 95.
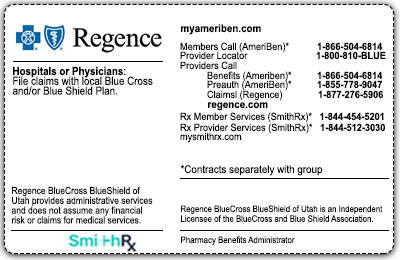
Meanwhile Medicare’s filing limit remains 12 months from the date of service, and traditional Indiana Medicaid has a 180-day filing limit.įor more information about the change, review Anthem’s Provider Communications article “ Reminder: Changes to timely filing requirements coming in October.” Indiana’s Medicaid Managed Care Entities also have a 90-day filing limit. The new 90-day requirement reflects Anthem’s commitment to “simplify processes, improve efficiencies, and better support coordination of care.” The change also aligns Anthem with other commercial payers, including Aetna, Cigna, and United Healthcare, all of whom have 90-day timely filing limits for claims. “One hundred eighty days has been the Anthem Blue Cross and Blue Shield (Anthem) standard since 2007,” the payer explained.
BCBS TIMELY FILING 2019 PROFESSIONAL
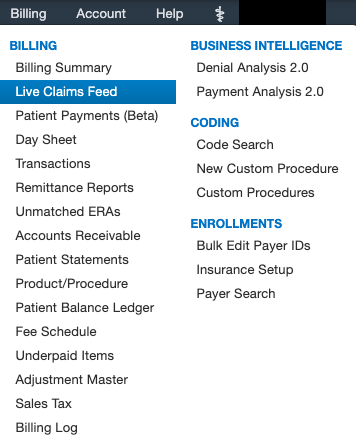
In 2016, when some professional and ancillary provider contracts inadvertently included a 90-day filing limit, Anthem issued a blanket correction, confirming their 180-day filing limit at that time. Beginning October 1, 2019, all claims will be subject to a 90-day filing requirement, and according to the payer, “Anthem will refuse payment if submitted more than 90 days after the date of service.”įor years, Anthem’s timely filing limit has been 180 days. Reach out insurance for appeal status.Anthem is changing their timely filing limit for professional claims. As of January 2019, a Medicare Advantage Open Enrollment Period is available. Wellmark BCBS of Iowa and South Dakota timely filing limit for filing an initial claims: 180 Days from the Date of service. Wellmark Blue Cross Blue Shield timely filing limit - Iowa and South Dakota. Services denied for failure to meet timely filing requirements are not subject to reimbursement unless the provider presents documentation proving a clean claim was filed within the applicable filing limit. If previous notes states, appeal is already sent. Anthem BCBS of Ohio, Kentucky, Indiana and Wisconsin timely filing limit for filing an initial claims: 90 Days form the date service provided. Claims filed beyond federal, state- mandated, or company standard timely filing limits will be denied as outside the timely filing limit.If we have clearing house acknowledgement date, we can try and reprocess the claim over a call.If claim history states the claim was submitted to wrong insurance or submitted to the correct insurance but not received, appeal the claim with screen shots of submission as proof of timely filing(POTF) and copy of clearing house acknowledgement report can also be used.
If the first submission was after the filing limit, adjust the balance as per client instructions.
BCBS TIMELY FILING 2019 CODE
The decision is deemed received on the date of delivery, if hand delivered, or, if mailed, on the earlier of the actual date of receipt or five days after deposit in the U.S. There is no timely filing limit on cancel claims (claim frequency code of 8). If claims submitted after the timely frame set by insurances, then those claims will be denied by insurance companies as CO 29-The time limit for filing has expired. We transmit decisions for out-of-state providers to the BCBS Plan in the provider's home state, and that BCBS Plan sends the decision to the provider. Timely Filing Limit is the time frame set by insurance companies and provider has to submit health care claims to respective insurance company within the set time frame for reimbursement of the claims.


 0 kommentar(er)
0 kommentar(er)
